What Is Endometriosis?
Understanding Symptoms, Hormones, and the Bigger Picture
23 Jan 2026

Quick Facts
- Endometriosis affects around 1 in 10 women and people assigned female at birth in the UK
- Diagnosis takes an average of 7–8 years
- Endometriosis is a systemic inflammatory condition
- Hormonal signalling plays a central role
- There is currently no cure but symptoms can be meaningfully managed
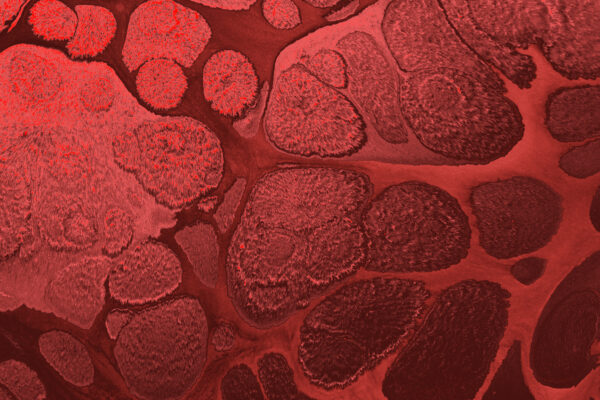
What Is Endometriosis?
Endometriosis is a chronic inflammatory condition where tissue similar to the lining of the uterus (the endometrium) grows outside the uterus, in areas where it doesn’t belong.
These endometrial-like cells are most commonly found within the pelvis – including the:
- Ovaries
- Fallopian tubes
- Pelvic ligaments
- Bowel
- Bladder
But can, more rarely, appear elsewhere in the body.
Despite resembling the uterine lining, this tissue behaves differently: it interacts with hormones, the immune system, and surrounding nerves in a way that drives inflammation, pain, and tissue scarring.
Endometriosis can affect individuals from adolescence onwards and may persist beyond reproductive years.
What’s Actually Happening in the Body?
During a typical menstrual cycle, the uterine lining thickens and sheds through menstruation.
In endometriosis:
- Endometrial-like tissue grows outside the uterus
- This tissue still responds to hormonal signals
- But it cannot shed or drain normally
As a result, each cycle can trigger:
- Local and systemic inflammation
- Accumulation of scar tissue
- Formation of adhesions, where organs bind together
- Sensitisation of pelvic nerves, amplifying pain over time
This explains why endometriosis pain may:
- Begin before bleeding starts
- Persist throughout the cycle
- Occur during ovulation, bowel movements, or sex
- Become chronic rather than purely cyclical
Common Symptoms of Endometriosis
Endometriosis is highly individual – symptom type and severity vary widely, and pain intensity does not reliably reflect disease stage.
Pain & Menstrual Symptoms
- Severe period pain (often described as sharp, stabbing, or burning)
- Pelvic pain that begins days before menstruation
- Chronic pelvic or lower back pain
- Pain during or after sex (dyspareunia)
- Pain radiating into the legs or hips
Heavy or Disruptive Bleeding
- Periods lasting longer than 7 days
- Heavy flow requiring frequent product changes
- Passing large blood clots
Over time, heavy bleeding can contribute to iron deficiency anaemia, leading to:
- Fatigue
- Hair thinning
- Breathlessness
- Feeling cold or light-headed
Bowel, Bladder & Systemic Symptoms
- Bloating or abdominal distension (“endo belly”)
- Constipation or diarrhoea, often cyclical
- Pain with bowel movements or urination
- Symptoms mimicking IBS or recurrent UTIs
- Persistent fatigue
- Low mood, anxiety, or emotional burnout linked to chronic pain
Painful periods are not normal. If symptoms interfere with daily life, work, or relationships, they warrant investigation.
Endometriosis and Hormones: The Oestrogen Connection
Endometriosis is widely recognised as an oestrogen-dependent condition.
Oestrogen Activity
Endometriotic lesions are capable of producing oestrogen locally.
This creates a self-sustaining inflammatory environment, encouraging lesion growth and pain signalling even when circulating hormone levels appear “normal.”
Progesterone Resistance
In a healthy cycle, progesterone helps regulate and stabilise the uterine lining.
In endometriosis, affected tissue often shows reduced responsiveness to progesterone, meaning oestrogen’s effects go unchecked.
This imbalance contributes to:
- Ongoing lesion activity
- Failure of tissue to regress
- Reduced effectiveness of certain hormonal treatments in some individuals
Endometriosis and Fertility
Endometriosis can impact fertility, with estimates suggesting 30–50% of people with endometriosis experience fertility challenges.
This may occur due to:
- Adhesions affecting fallopian tube function
- Ovarian cysts (endometriomas) impacting ovarian reserve
- Inflammatory changes affecting egg quality or implantation
Importantly, many people with endometriosis do conceive naturally, particularly when the condition is identified and managed early.
How Is Endometriosis Diagnosed?
Diagnosis remains challenging due to symptom overlap with other conditions such as IBS, fibroids, adenomyosis, or PCOS.
Assessment may include:
- Detailed symptom history
- Pelvic examination
- Ultrasound or MRI (useful for deep or advanced disease)
- Laparoscopy, a minimally invasive surgical procedure, which remains the gold standard for definitive diagnosis
While surgery confirms diagnosis, blood markers and hormone testing can provide valuable early insight, guide referrals, and help rule out contributing or overlapping conditions.
Living With Endometriosis: Management Options
There is currently no cure for endometriosis, but many people experience significant symptom improvement with the right support.
Management may include:
- Hormonal therapies (e.g. progestins, contraceptives, GnRH analogues)
- Pain management strategies
- Surgical excision in selected cases
- Nutritional and lifestyle interventions
- Pelvic physiotherapy
- Psychological support for chronic pain
We take a whole-body approach – recognising the roles of inflammation, hormone metabolism, nutrient status, thyroid health, and immune balance in shaping symptom severity and resilience.
Final Thoughts
Endometriosis is real, common, and complex – but it is not something you have to endure without answers.
If you’re experiencing persistent pelvic pain, heavy bleeding, fatigue, or cyclical bowel or bladder symptoms, early investigation matters.
With personalised insight and informed care, it’s possible to reduce symptom burden, protect fertility, and improve long-term wellbeing.
Understanding what’s driving your symptoms is the foundation of effective support.
Latest Insights
Stay up to date with latest research, tips and trends in health and nutrition.