Ovarian Ageing
Understanding Fertility, Hormonal Change, and Long-Term Health
23 Jan 2026

Quick Facts
- Ovarian ageing begins before birth – Females are born with a finite number of eggs, which gradually decline in both quantity and quality over time.
- The rate of decline accelerates after the mid-30s
- Shifts in ovarian function affect metabolism, bone health, mood, cardiovascular risk, and cellular ageing.
- Some people experience few noticeable changes, while others develop significant physical or emotional symptoms.
- Menopause marks the end of ovarian function – not the start of ageing
What Is Ovarian Ageing?
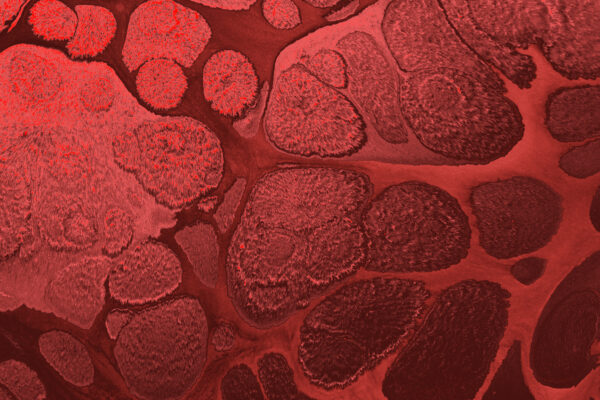
Ovarian ageing refers to the natural, gradual decline in both the number and quality of a woman’s eggs over time.
Unlike other tissues in the body, the ovaries contain a finite supply of follicles established before birth.
These follicles are steadily lost throughout life and cannot be replenished.
Alongside the reduction in egg number, the remaining eggs experience age-related changes in genetic stability and cellular function, which contributes to declining fertility and, eventually, the transition into menopause.
Who Does Ovarian Ageing Affect?
Ovarian ageing affects all women – it is a universal biological process, not a condition or disease.
- The decline begins before birth, with a gradual loss of follicles throughout childhood and adulthood
- Around the mid-30s, the rate of decline accelerates
- Hormonal fluctuations become more noticeable during the perimenopausal years
- By approximately age 50, ovarian function typically ceases, marking menopause
The timing and pace of this process vary considerably and are influenced by genetics, health history, lifestyle factors, and environmental exposures.
Common (Surface-Level) Symptoms
Not everyone experiences symptoms in the same way. Some may notice subtle changes, while others experience more pronounced disruption.
1. Changes in the Menstrual Cycle
Periods may become irregular, shorter, longer, heavier, or unpredictable as ovarian hormone production fluctuates.
2. Vasomotor Symptoms (Hot Flushes)
Sudden waves of heat, flushing, and sweating can occur due to altered thermoregulation linked to oestrogen decline.
3. Sleep Disturbances
Difficulty falling asleep, staying asleep, or early waking — often worsened by night sweats or hormonal shifts.
4. Mood Changes
Increased irritability, anxiety, low mood, or emotional volatility may emerge as hormones that influence neurotransmitters change.
5. Pelvic Floor Changes
Reduced oestrogen can weaken pelvic tissues, contributing to urinary leakage, pelvic heaviness, or discomfort.
6. Vaginal Dryness
Changes in vaginal lubrication and tissue elasticity may lead to discomfort during intimacy or daily activities.
What’s Happening Beneath the Surface?
Beyond visible symptoms, ovarian ageing drives complex cellular and molecular changes that influence long-term health.
Cellular & Molecular Changes
- DNA Integrity
- Lower oestrogen reduces cellular protection against oxidative stress, increasing susceptibility to DNA damage.
- Inflammatory Shifts
- Chronic, low-grade inflammation may rise, influencing joint health, metabolic function, and cardiovascular risk
- Metabolic Changes
- Hormonal shifts can affect glucose handling and fat metabolism, contributing to weight changes and insulin resistance.
- Epigenetic Alterations
- Changes in hormone signalling can influence how genes are switched on or off, shaping ageing trajectories and disease risk.
- Mitochondrial Function
- Declining efficiency in cellular energy production can contribute to fatigue, reduced resilience, and slower recovery.
- Antioxidant Imbalance
- Reduced endogenous antioxidant activity leaves cells more vulnerable to oxidative damage.
- Endocrine System Changes
- Alterations in oestrogen, progesterone, and related hormones impact nearly every system — from bone density to mood regulation.
- Telomere Dynamics
- Accelerated telomere shortening may occur, influencing cellular ageing and tissue repair capacity.
These internal shifts explain why ovarian ageing affects far more than reproductive health alone.
Anti-Müllerian Hormone (AMH) and Ovarian Ageing
Anti-Müllerian Hormone (AMH) is one of the most widely used markers for assessing ovarian reserve – a reflection of the number of follicles remaining in the ovaries.
AMH is produced by small, developing follicles and tends to decline steadily with age, making it a useful indicator of where someone may sit along the ovarian ageing trajectory.
What AMH Can Tell Us
Follicle quantity, not egg quality
AMH provides insight into the number of remaining follicles, but it does not assess egg quality, which also declines with age.
Earlier insight than cycle changes
AMH often begins to fall years before menstrual irregularity appears, making it valuable for early fertility planning.
Predictive for ovarian response, not natural fertility alone
AMH helps estimate how the ovaries may respond to stimulation (e.g. in IVF), but it does not reliably predict the ability to conceive naturally in any given cycle.
Individual variability matters
Two people of the same age can have very different AMH levels, influenced by genetics, ovarian surgery, endometriosis, chemotherapy, and lifestyle factors.
How AMH Changes Over Time
- AMH is highest in early adulthood
- Levels gradually decline through the 30s
- The rate of decline often accelerates during the late 30s and early 40s
- AMH becomes very low or undetectable approaching menopause
Importantly, a lower AMH does not mean pregnancy is impossible – it simply reflects reduced ovarian reserve.
AMH in Clinical Context
AMH is most informative when interpreted alongside other markers, including:
- Follicle-stimulating hormone (FSH)
- Luteinising hormone (LH)
- Oestradiol
- Menstrual history and cycle regularity
- Symptoms of perimenopause or hormonal change
Viewed in isolation, AMH can be misleading.
In context, it provides valuable insight for fertility planning, hormone health assessment, and personalised care pathways.
Final Thoughts
Ovarian ageing is a natural biological process, but its impact extends well beyond fertility and menopause.
The hormonal and cellular changes that occur during this transition influence energy, mood, metabolism, bone health, and long-term disease risk.
Understanding what’s happening beneath the surface allows for earlier awareness, informed decision-making, and proactive support – whether your goal is fertility planning, symptom management, or protecting long-term health.
Ageing is inevitable; how we navigate it can be personalised.
Latest Insights
Stay up to date with latest research, tips and trends in health and nutrition.